Lessons Learned from University of Nevada Las Vegas (UNLV):
Engage Your Team and Discuss Your Workflow
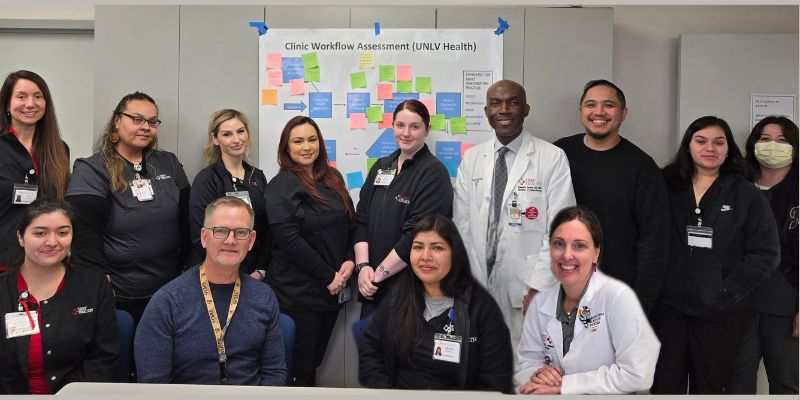 Back row (left to right): Lisa Contreras, Sandy Pene, Nancy Delcid, Katherine Mercado, Kyanne Sevedge, Dr. Kenneth Izuora, Dino De Jesus, Yadira Yanez Rodriguez, Virginia Virula.
Back row (left to right): Lisa Contreras, Sandy Pene, Nancy Delcid, Katherine Mercado, Kyanne Sevedge, Dr. Kenneth Izuora, Dino De Jesus, Yadira Yanez Rodriguez, Virginia Virula.
Front row (left to right): Jasmine Velasquez, Robert Swaim, Michelle Uriostegui Fierro, Dr. Amber Champion.
Not pictured: Maryann Sivongxay, Jocsan Ordinario, Christine Rios and Sheila Barela.
UNLV’s Endocrinology Department and its vaccination QI efforts are led by Kenneth Izuora, MD, FACE. When UNLV reviewed vaccination rates among their patients with diabetes and found them to be suboptimal, Dr. Izuora used a team-based approach to help identify reasons for the gaps and explore potential solutions.
With support from a supplemental CDC grant made available through the SSAAI Project, Dr. Izuora worked with AACE to analyze his clinic’s workflow with the goal of improving vaccination rates among patients with diabetes. The project involved a root cause analysis and creating a flowchart representing the current process during a typical clinical encounter.
Everyone on the team – clinical and administrative staff - contributed and participated in the process.
The UNLV team came together for an afternoon and talked about their current workflow and how processes could be changed in order to integrate the CDC’s Standards for Adult Immunization Practice (SAIP). This meant the team would be modifying their workflow to incorporate each CDC Standard, which calls for health care providers to Assess, Recommend, Refer, Administer, and Document vaccines.
Using a poster size version of their current workflow, the UNLV team reviewed their processes and generated ideas for changes. As each idea was discussed, the team member who raised it wrote the idea on a post-it note and applied it to the relevant process on the workflow poster. Using different post-it note colors for each SAIP, a new, colorful workflow began to emerge.
The team talked about potential challenges that could impact the application of their new workflow ideas, with the most significant being delays. According to Dr. Izuora, the team looked at it from the point of view of where they could make the most impact with the least time added.
Solutions began to emerge, and the team focused on those changes that would occur before or after the clinic visit. For example, they could begin to routinely assess and reconcile the vaccine status of patients with the Nevada IIS prior to the visit and during check-in and rooming. For those changes that would be implemented during the clinic visit, the team thought it would be best to work on one change at a time.
View the before and after versions of UNLV’s workflow.
The UNLV Endocrine Care team is now using their modified workflow and implementing QI interventions to help improve vaccination rates for their patients with diabetes. The team continues to be involved, not only by working on planned changes to their workflow but also providing feedback on the changes to help make modifications, as necessary, to help ensure future success and sustain changes.
Dr. Izuora believes that engagement of the team from the earliest phases helped all staff have a sense of ownership, which led to motivation to contribute to identifying and implementing solutions. The team-based approach was, and continues to be, critical to success.
Here are Three Take-away Tips from Dr. Izuora and his team:
- It takes a TEAM to make and sustain change. When the team is involved in identifying solutions, they can share concerns about challenges they anticipate and work with other team members to address them. Tackling potential problems in the “build” of a new workflow can help make that workflow really flow!
- Use QI tools and resources. Fishbone diagrams can help you understand “why” a gap exists. Workflow analysis tips and tools will help you identify how best to make effective and efficient changes. There are many available and there is no need to reinvent the wheel.
- Be open to workflow changes. You might be surprised by how some changes can be implemented with more efficiency that you think!
If you are interested in leading your own QI intervention to improve vaccination coverage among your adult patients with diabetes, visit AACE’s website and consider using QI tools from the Institute of Healthcare Improvement (IHI). The IHI’s Quality Improvement Essentials Toolkit is a free resource that can help you identify, plan, and measure improvements. Here are some recommended resources and tools from Dr. Izuora based on UNLV’s work:
- Fishbone (Cause & Effect) Diagram
- Using Clinical Workflow Analysis to Enhance eHealth Implementation Planning: Tutorial and Case Study
- AHRQ Workflow Analysis Educational Presentations
- AHRQ Searchable Database of Workflow-Related Publications
Let AACE know if you embark on a vaccination QI effort and on what you learn!
